Taking on some of the most common questions (and myths) about
There’s a lot of information out there about . We hear it from our friends, our siblings, our doctors, our mothers, and our internet searches. While much of this information is good, some of it is not entirely true or not true for everyone — and some of it is completely bunk.
Our bodies are complex, so it’s hard to label every claim about as either true or false. Still, we think it’s important to challenge and investigate claims we’ve heard to see which are backed up by evidence, and which aren’t! Here are some of the most common questions we’ve asked and been asked about , and what the real answers are.
Can I still get pregnant while on ?
Technically, yes, this one’s true: You can still get pregnant while on . The likelihood of getting pregnant while on depends on which method you’re using, and whether you’re using it perfectly (you’ll sometimes hear this called “perfect use.”) Think of perfect use as the condom that stays in place, doesn’t tear, and doesn’t leak.
If you’re using like the pill, IUDs, or contraceptive implants — methods rated as highly effective, especially for typical use and not just perfect use — it’s unlikely you’ll get pregnant. If you want to decrease your odds of pregnancy even further, you can combine methods, for example by adding condoms and/or pulling out to a hormonal method like the pill, the patch, the shot, or an IUD.
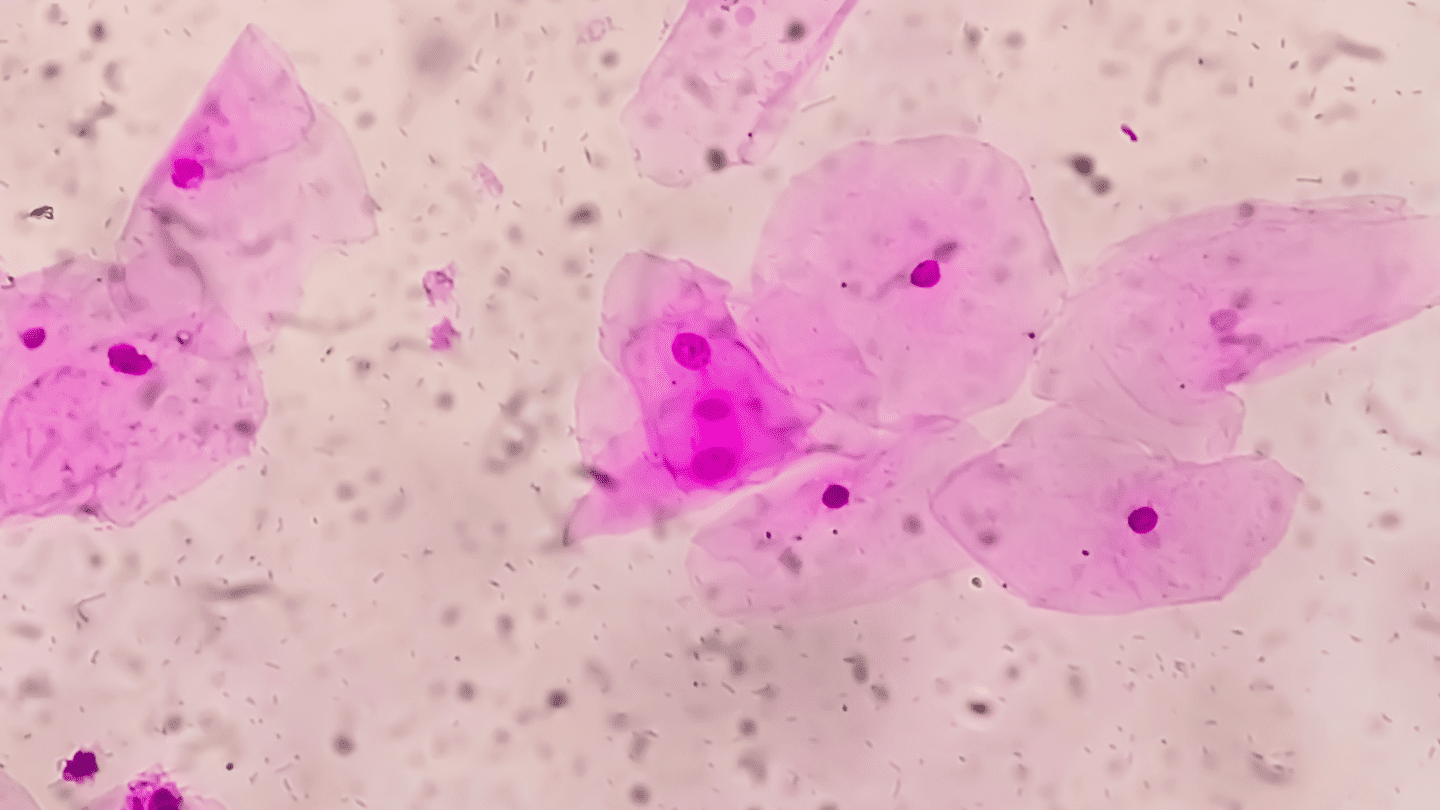
Does the pill protect me from sexually transmitted infections?
No, hormonal birth controls like the pill do not protect against sexually transmitted infections. The only way to protect against STIs and STDs during sexual contact is to use a condom.
According to the CDC, using condoms consistently and correctly is the best way to protect against sexually transmitted infections like HIV and other STDs.1 They’re most effective against diseases that are transmitted through bodily fluids, like chlamydia and gonorrhea. Other STDs are transmitted just by skin-to-skin genital contact, and this can still occur even with even a properly worn condom. Although condoms do offer some protection against these, you’re not as protected against STDs like genital herpes, or human papillomavirus (HPV).
Like what you’re reading? Get the latest straight to your inbox 💌
Is the pill effective immediately after you begin taking it?
No, the combination pill can take up to seven days to start preventing pregnancy.2 So, you should plan on using another form of if you’re having sex during that time. It depends when during your cycle you start taking it, though — if you start during your period (specifically, within five days of the first day of your period), you’ll be protected right away.2 And if you’re taking the pill for other benefits, like to relieve acne,3 it can take as long as three cycles (up to three months) to see those benefits as your body’s hormones adjust to new levels.
Will make me gain weight?
The answer to this question is no, for most types of contraceptives at least. Studies of weight gain and hormonal contraceptives dating back decades find that options like the pill, IUD, ring, and patch don’t cause weight gain. But two kinds of hormonal birth control, the shot, also called Depo-Provera, and the implant, can cause some people, but not all, to gain weight.
That will make you heavier is a super commonly held belief, and it’s a side effect many hormonal contraceptive users attest to. In a survey of more than 2,500 women, 69% reported having experienced at least one side effect; of them, 55% reported weight gain and 41% said it was noteworthy enough that they stopped using the contraceptive because of it.4
Yet when researchers look for a direct effect of most hormonal contraceptives on weight gain, they can’t find it. In 2014, researchers reviewed 49 clinical trials that tested the idea, and found no consistent evidence that the combined contraceptive pill causes weight gain.5
What gives? Some researchers suspect temporary water retention is to blame, or possibly an increase in appetite.6 But these theories don’t have much evidence behind them yet — more research is needed to figure out if there is really a link and why.
There is evidence that the birth control shot and the implant can lead to weight gain for some people. A 2019 review of research on Depo-Provera reports a number of studies found weight gain to be a side effect.7 A 2014 study of both Depo and the implant also found that users of those two methods gained more weight than those using hormonal and copper IUDs (though the implant showed no evidence of increased weight gain after adjusting for age and race.)8
Is adyn right for you? Take the quiz.
It may be that only some people gain weight when using the shot or implant, though. One 2020 study in the journal Contraception notes that some genetic s might predispose people to weight gain when using the implant.9 A 2009 study of Depo-Provera users also found that some people gained significantly more weight than others after starting the contraceptive.10
Those two methods aside, the evidence shows the pill, IUDs and other common forms of won’t cause weight gain.
Will using prevent me from getting pregnant in the future? Will it cause ?
No! Reversible forms of do not make you infertile or decrease your chances of having a baby someday. If you’re using like oral contraceptives, your fertility should return to normal levels within 2–6 months, although some people can get pregnant immediately.7 In fact, one study found that women coming off the pill after more than two years of use were actually more likely to get pregnant than compared to their peers who had used only barrier methods before trying to get pregnant.7
Read more: Can cause ?
Will “unbalance” my hormones?
No, in fact, the opposite is typically true! Hormonal can help regulate the extreme changes in levels that occur during your menstrual cycle, which, for some people, is a good thing. Regulating your hormones out can help with heavy or irregular bleeding, cramping, and more. levels naturally fluctuate (“balanced” hormones isn’t really a thing), and they continue to fluctuate even when you’re on .
Why take if you’re not sexually active?
There are a number of benefits to beyond preventing pregnancies, and many people take hormonal contraceptives for other reasons. Because can help to even out hormonal fluctuations, it can help with things like PMS symptoms, irregular bleeding, , and even acne.9
Will make me depressed?
This one depends on your biology. Certain methods of are associated with higher risk of depression, especially in adolescents.10-11 and , two of the key hormones in many hormonal birth controls, affect your mood. But that doesn’t automatically mean will make you depressed. For some people, can actually improve mood by keeping cycle-related irritability and moodiness in check. But for others, it can have the opposite effect: Mood changes are one of the most frequently cited reasons that people stop taking .
This is a topic that desperately needs more study. We hope you’ll join us here at adyn as we develop a more complete data set on side effects like depression, in search of more inclusive scientific conclusions!
Will my IUD fall out?
No, it’s not likely that your IUD would fall out — though it is possible. The IUD expulsion rate can range from 2–10% depending on age and how long the device is left in place.12-14 Some researchers have found it tends to be higher for teens and for people who have had one in place for longer. But a lot of studies have reported conflicting results, so more research is needed.
Be sure to occasionally check that your IUD strings are still in place, and if anything ever seems amiss or if you know your IUD has fallen out, contact your doctor right away and use alternative forms of to be safe.
Are all methods effective?
All forms of , when used correctly, do something to reduce your risk of pregnancy. But not all forms of are equally effective. We only recommend using contraceptives rated : 98% effective for preventing pregnancy with perfect use. Birth control shots, patches, pills, rings, implants, and IUDs all fall into this category.
Do you still need if you practice fertility awareness?
Yes. Fertility awareness is not considered an effective form of . We recommend switching to or supplementing with another method if you don’t want to get pregnant.
That said, if you’re ovulating (so, not taking ), it can be helpful to know which times of the month you’re most and least likely to get pregnant. Most ovulating people are at their most fertile in the five days before ovulation until one day after. Ovulation occurs around day 14 of your menstrual cycle, counting from when your period starts. That means you can decrease your chances of pregnancy by avoiding penis-in-vagina sex on days 10 through 15 of your cycle.
Do you still need if your partner pulls out?
Yes. The pull-out method is not considered an effective form of , and you should supplement it with additional contraceptives if you don’t want to get pregnant. Pulling out, also called the “withdrawal method,” is only about 82% effective at preventing pregnancy.15 That means nearly 1 in 5 couples using that strategy will get pregnant every year. The reason it’s not effective is twofold: it’s hard to actually achieve, and even when your partner pulls out on time, pre-ejaculate can contain sperm.16
Will all methods affect my hormones?
No, not all methods affect your hormones. Although some options use hormones to prevent your body from ovulating, others use physical barriers and other methods. Internal and external condoms (aka “male” and “female” condoms), and other barrier methods won’t affect your hormones, nor will spermicidal gels. That said, these methods aren’t as effective as methods like the pill, patch, ring, implant, or hormonal IUDs. One notable highly effective, non-hormonal option is the copper IUD, which works by preventing sperm from swimming properly.17
Any other myths you want fact checked? Tweet at us with your question or a myth that needs busting!
This article was originally published on January 24, 2022 and updated on May 9, 2024.
-
- CDC. Condom Fact Sheet in Brief. Last updated 2021 Sep 14. Last accessed 2022 Jan 17.
- Planned Parenthood. Are Birth Control Pills Effective? N.D. Last accessed 2022 Jan 17.
- Harper, Julie C. “Use of oral contraceptives for management of acne vulgaris.” Dermatologic Clinics 34 (2016): 159-65.
- Gallo, Maria F., et al. “Combination contraceptives: effects on weight.” Cochrane Database of Systematic Reviews 1 (2014).
- Madden, Tessa, et al. “The role of contraceptive attributes in women’s contraceptive decision making.” American Journal of Obstetrics and Gynecology 213.1 (2015): 46-e1.
- Cagnacci, Angelo, and Anna Biasioli. “The Effect of Hormonal Contraceptives on Metabolism.” Female and Male Contraception. Springer, Cham, 2021. 299-317.
- Mikkelsen, Ellen M., et al. “Pre-gravid oral contraceptive use and time to pregnancy: a Danish prospective cohort study.” Human Reproduction 28.5 (2013): 1398-1405.
- Mayo Clinic Staff. Hirsutism. MayoClinic.org. 2021 Oct 12. Last accessed 2022 Jan 19.
- Słopień, Radosław, et al. “Use of oral contraceptives for management of acne vulgaris and hirsutism in women of reproductive and late reproductive age.” Przeglad Menopauzalny (Menopause Review) 17.1 (2018): 1.
- McKetta, Sarah, and Katherine M. Keyes. “Oral contraceptive use and depression among adolescents.” Annals of Epidemiology 29 (2019): 46-51.
- Keenahan, Laura, et al. “Rates of intrauterine device expulsion among adolescents and young women.” Journal of Pediatric and Adolescent Gynecology 34.3 (2021): 362-365.
- Skovlund, Charlotte Wessel, et al. “Association of hormonal contraception with depression.” JAMA Psychiatry 73.11 (2016): 1154-1162.
- Diedrich, Justin T., David A. Klein, and Jeffrey F. Peipert. “Long-acting reversible contraception in adolescents: a systematic review and meta-analysis.” American Journal of Obstetrics and Gynecology 216.4 (2017): 364-e1.
- Rivera, R., M. Chen-Mok, and S. McMullen. “Analysis of client characteristics that may affect early discontinuation of the TCu-380A IUD.” Contraception 60.3 (1999): 155-160.
- Kost, Kathryn, et al. “Estimates of contraceptive failure from the 2002 National Survey of Family Growth.” Contraception 77.1 (2008): 10-21.
- Killick, Stephen R., et al. “Sperm content of pre-ejaculatory fluid.” Human Fertility 14.1 (2011): 48-52.
- Planned Parenthood. What are non-hormonal IUDs? N.D. Last accessed 2022 Jan 19.