The pill, the patch, the ring, the shot, the morning after pill, the IUD — there are so many forms of available, each with their own advantages and potential drawbacks.
While it can seem overwhelming to choose the that is right for you, many forms of work in similar ways — by providing synthetic reproductive hormones. To manage your health, it’s important to understand how works and how it interacts with natural hormones in the reproductive system.
How Hormones Work
Hormones are chemical messengers—they are created and released by endocrine organs and act elsewhere in the body on other organs or tissues. The major endocrine glands include the pituitary gland, thyroid, adrenal glands, pancreas, , and testes.
Most hormones travel in the body through the bloodstream or in the fluid that surrounds cells. Each primarily impacts the cells that have receptors specific for that . There are around 50 hormones in the human body1, each with their own roles in physiological functions. Hormones control everything from growth and development to mood.
Reproductive hormones are those involved in fertility and sexuality.2 Reproductive organs produce varying levels of the reproductive hormones depending on a person’s age, reproductive status and general health. Some of the major reproductive hormones are gonadotropin releasing , , , , and .
Hormones and the Menstrual Cycle
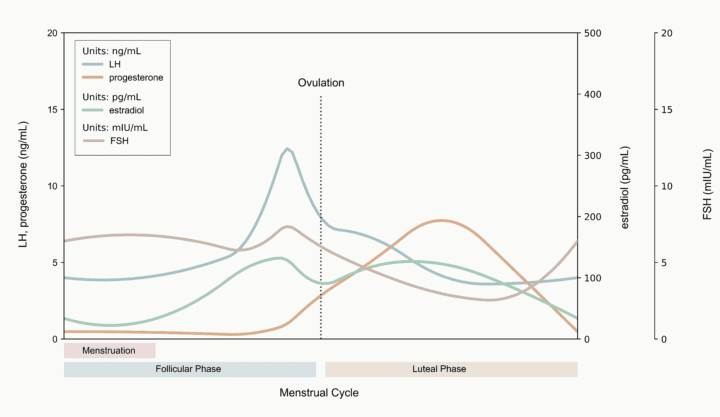
Reproductive hormones influence the menstrual cycle.3 When someone with reaches puberty, gonadotropin releasing triggers the pituitary gland to produce two hormones, () and ().4
FSH and are responsible for the development and maturation of follicles (fluid-filled ‘sacs’ that contain eggs), and ovulation (the release of a mature egg from the follicle).5 In response to increasing levels of from the , a surge in triggers ovulation. Once an egg is released from the ovary, the empty follicle continues to produce , and now also produces , which are needed to prepare the for possible pregnancy.5
If the released egg does not become fertilized and implant in the , the lining of the is shed in a withdrawal bleed or period. This sequence of events occurs roughly every month and is called the menstrual cycle. Hormones drive physiological changes during different phases of the menstrual cycle3:
Phase 1: The Menses Phase
The menses phase is when your body sheds the extra endometrial lining it had prepared for a possibly fertilized egg. In other words, it is when you have your period. At the beginning of the menses phase, and levels are low. These levels dropped at the end of the previous cycle. This drop is what causes your period or withdrawal bleed, which typically lasts 3-7 days.
Phase 2: The Follicular Phase
As a new cycle begins, the low levels of and cause increased production of and from the pituitary gland. As these pituitary hormones rise, they stimulate the to increase production. The primary produced by the during the follicular phase is an called estradiol, and a smaller amount of is also produced. These changes result in the recruitment of ovarian follicles that begin to mature.3
Phase 3: The Ovulation Phase
At the end of the follicular phase, the rising levels of estradiol and trigger a surge of production by the pituitary gland. This rapid rise in causes ovulation, the release of a mature egg from a follicle– only one follicle matures completely and releases an egg. The released egg moves from the ovary to the fallopian tube and towards the .
Phase 4: The Luteal Phase
The luteal phase occurs after the egg has been released from the follicle. Changes occur that would prepare a for a pregnancy if the released egg becomes fertilized. The empty follicle continues to produce both estradiol and , but the now high levels of primarily drive the physiological changes in the luteal phase.
These rising levels thicken the uterine lining in preparation for possible pregnancy. The thickening of the uterine lining is necessary for a fertilized egg to implant. If an egg isn’t fertilized and implanted in the , the empty follicle stops producing estradiol and . As these levels decrease, the menses phase is triggered, and the cycle starts all over again.3,5
A quick caveat: The changes discussed here are what is “typical” for someone with prior to . However, due to medical conditions like PCOS or , high or low body weight, stress, , and a number of other factors, menstrual cycle patterns can vary quite a bit across individuals and over time.
Like what you’re reading? Get the latest straight to your inbox 💌
Hormonal and s
The name (aka ) is fairly self-explanatory — it works to prevent pregnancy before it happens. There are many methods of . Today we are going to focus on hormonal methods and how hormones and interact. But first, here is a quick overview of the various kinds of hormonal and options.
Is adyn right for you? Take the quiz.
Non-hormonal
Non-hormonal methods contain no hormones and are available to those who prefer not to use hormones because of personal preference or medical necessity. They include:
- Tubal ligations
- Vasectomies
- Condoms
- Cervical caps
- Diaphragms
- The rhythm method
- Copper IUD
- Vaginal gel
These have varying degrees of effectiveness, from 78%-99.9%, with typical use.6
There is currently one type of non-hormonal IUD available in the US. This IUD prevents pregnancy with copper, a super-effective spermicide that interferes with sperm transport, egg fertilization and possibly prevents egg implantation7, all without harming the person with the IUD.
Hormonal
Hormonal methods contain an and a or only a . They include:
- Combined pill
- Progestin-only pill
- The patch
- The ring
- The shot
- All other IUDs
- The morning-after pill (emergency contraception)
Just like non-hormonal methods, hormonal birth controls also have varying degrees of efficacy.6
How Do Hormonal Birth Controls Work?
While each method has a slightly different mechanism of action, there are a few key, common mechanisms that work to prevent pregnancy. Some of these mechanisms are8:
- Preventing ovulation
- Thickening cervical mucus
- Changing the uterine lining
Many types of prevent ovulation from occurring. Therefore, they stop a potential pregnancy early on in the process– if no egg is released from the ovary, no egg can be fertilized!
Options for combined birth control pills
While the ways they work are generally similar, birth control pills are not all the same. They come in different formulations, with different doses and specific synthetic hormones.
Of the birth control pills that contain both an and a (combined oral contraceptives), there are monophasic, biphasic, and triphasic pills.8 and progestin-containing birth control pills work primarily by preventing ovulation, but they also can impact the uterine lining and cervical mucus to prevent implantation and fertilization.9
- Monophasic pills have the same amount of hormones in every pill, save for the week, when the pill contains no hormones. You are still protected from pregnancy during this time, as the pill has prevented ovulation, so there is no egg to be fertilized.8
- Biphasic and triphasic pills have different doses of the and that mimic the changes that occur during the menstrual cycle.8
Other options
- The mini pill – A less commonly used birth control pill called the “mini pill” contains only a . It primarily works by thinning the lining of the and thickening the cervical mucus. In some people, it can also prevent ovulation.10 For this pill, there is no week, which often results in periods stopping over time.
- The patch and the ring – Both of these work in a similar way and contain an and a . Both release hormones for three weeks and are removed for one week to trigger a withdrawal bleed. Whereas the ring is inserted into the and hormones are absorbed vaginally, the patch is put on the upper body (the arm, abdomen, or buttock) and hormones are absorbed through the skin.8
- The shot, hormonal IUDs, and the implant (Nexplanon) – These longer-acting methods of contain only a progestin6. The in the implant or IUD is released continuously over the period of a few years. The shot (Depo-Provera) is administered every three months. These progestin-only methods work by thinning the uterine lining and making cervical mucus thicker, preventing implantation and fertilization, and, in some people, also inhibiting ovulation.8
- Emergency contraception – Plan B emergency contraception also is a progestin-only contraceptive. Levonorgestrel, the found in Plan B emergency contraception, is the same found in hormonal IUDs and many formulations of combined birth control pills.11 Emergency contraception can work at any point during the menstrual cycle because it helps prevent 1) the release of an egg from the ovary, 2) a released egg from being fertilized, and 3) a fertilized egg from attaching to the uterine lining. Plan B emergency contraception works best the sooner it is taken to when unprotected sex occurred.
Your Hormones on
Understanding how hormones and interact is important for understanding our bodies and our health. Now that you understand your hormones during your menstrual cycle and how they work in hormonal birth controls, you are ready to make your own precise choice, and adyn is here to help.
-
- E.Hormone: A Gateway to Environmental Signaling. Endocrine System: Types of Hormones. Tulane University. (2020). http://e.hormone.tulane.edu/learning/types-of-hormones.html. Accessed 08/2021-10/2021.
- National Cancer Institute. Reproductive Hormones. NCI Dictionary. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/reproductive-hormone. Accessed 10/2021.
- Reed BG, Carr BR. The Normal Menstrual Cycle and the Control of Ovulation. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext. South Dartmouth (MA): MDText.com, Inc. https://www.ncbi.nlm.nih.gov/books/NBK279054/ [Updated 2018 Aug 5]. Accessed 04/2021 to 10/2021.
- Breehl L, Caban O. Physiology, Puberty. In: StatPearls. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534827/ [Updated 2021 Apr 21]. Accessed 04/2021 to 10/2021.
- University of California, San Francisco. The Menstrual Cycle. Patient Education, UCSF. https://www.ucsfhealth.org/education/the-menstrual-cycle. Accessed 10/2021.
- Planned Parenthood, (n.d.). Birth control methods & OPTIONS: Types of birth control. https://www.plannedparenthood.org/learn/birth-control. Accessed 04/2021- 10/2021.
- ParaGard drug label insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/018680s069s070lbl.pdf. Revised 09/2019. Accessed 10/2021.
- Institute for Quality and Efficiency in Health Care. (2006). Contraception: Hormonal contraceptives. InformedHealth.Org. https://www.ncbi.nlm.nih.gov/books/NBK441576/ Updated 2017 June 29. Accessed 04/2021 to 10/2021.
- American College of Obstetricians and Gynecologists. (2021). Combined Hormonal Birth Control: Pill, Patch, and Ring. ACOG. https://www.acog.org/womens-health/faqs/combined-hormonal-birth-control-pill-patch-ring. Accessed 04/2021 to 10/2021.
- American College of Obstetricians and Gynecologists. (2021). Progestin-Only Hormonal Birth Control: Pill and Injection. ACOG. https://www.acog.org/womens-health/faqs/progestin-only-hormonal-birth-control-pill-and-injection
- Planned Parenthood. What’s the Plan B morning-after pill? https://www.plannedparenthood.org/learn/morning-after-pill-emergency-contraception/whats-plan-b-morning-after-pill. Accessed 10/2021.








