As a company working on improving the experience, we naturally are categorized as a “women’s health” company. The realm of women’s health takes many names and they often are used interchangeably: reproductive health, menstrual health, sexual health. While all of these labels can apply, they do not tell the whole story.
Hormonal birth control users are incredibly diverse in identity. Any race, age, ability, class, sexuality, or gender, hormonal birth control users share similar reproductive anatomy — and . We commit to being as inclusive as we can for our diverse community.
At adyn, we know how powerful language is. Our understanding of the world is created through language, and we connect through conversations. Because of this, the way we talk about things and with people is important.
Untangling Sex and Gender
While they will align for some people, sex and gender are different identities, defined by two different parameters.
- Sex: Legal sex (in most states) is restricted to male or female. This is assigned to a child at birth by a doctor, most often based on the child’s external anatomy. However, this designation of sex is an oversimplification and ignores intersex individuals who biologically exist outside the binary of male and female. This is a variation that occurs naturally in humans (estimated to occur in 1-2 out of every 100 people born in the U.S.). Intersex people may have combinations of sex chromosomes that are different than XY and XX, like XXY. Other intersex people have different combinations of genitals or internal sex organs — such as a person with both ovarian and testicular tissues.
- Gender is determined by someone’s personal internal experience and how they choose to name it. For many, it takes time to explore and understand their gender identity enough to choose or create language that fits the way they feel. For some, the words they use to identify their gender may change over time. Identity might not be fixed, but every individual has the right to define themselves.
At birth, it is usually assumed that a person’s gender will align with their sex and their gender expression will align with gendered expectations. In reality, gender is more fluid than that.
A Nuanced Understanding of Anatomy and Gender Identity
When we think about our place in the “women’s”, “female”, “reproductive”, “menstrual” health world, we go back to our foundation in precision medicine. We know that no solution is “one-size-fits-all”, the same way that we know no label is one-word-fits-all.
At adyn, we strive to create a shared language with our community that reflects us and honors all of our unique journeys. Our language choices, just like everything else we do, takes into consideration the individual and their unique story to provide the best care possible.
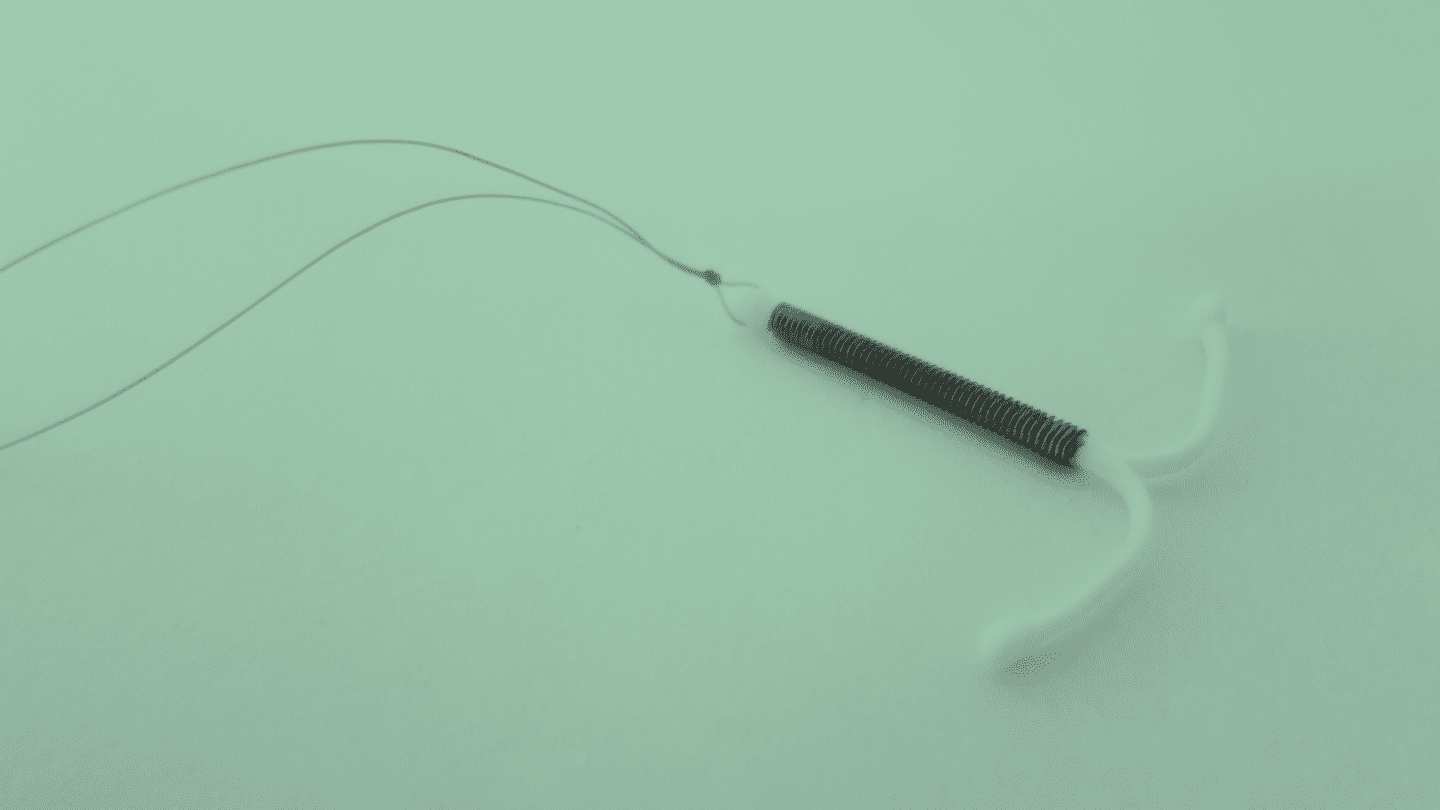
Hormonal birth control users share anatomical traits like ovaries, uteri, and vaginas. We may refer to them as “people with a ”, “people with ”, or “pregnant-capable people”. Hormonal birth control users share experiences like menstruation. We may refer to them as “people who menstruate” or “people with (menstrual) cycles”.
Many people may just say “women” to describe this demographic. It’s true that many women can share the same anatomical traits and live similar experiences, but we know that’s not the case for all.
Not all women have a or , even if they were born with that anatomy. This may be because of surgeries like a (the second most common surgery among people born with a ) or . Similarly, not everyone with a or are women. Transgender men and people across the gender spectrum may have a or , and even a menstrual cycle.
30 Years on
Outside of gender, users are diverse in age. On average, people with uteri may be on for 30 years of their life, starting as early as their first menses. That means our community includes people who are, by age, not women, but rather teenagers and children.
They have different needs, goals, and considerations than people who are older, and we should recognize that. The label “women” doesn’t encompass the younger demographic within our community in a way that allows us to provide the best care. Saying, “women and people [with a /, who menstruate, with cycles]”, or “birth control users” better encompasses our entire community.
Like what you’re reading? Get the latest straight to your inbox 💌
Gender Erasure in Scientific Research
While we strive to make our language as inclusive as possible, we exist in a world that is not. adyn is data-driven and evidence-based, and we utilize peer-reviewed research to provide context to our own work.
Just as we know that there are glaring gaps in medical research between men and women, the gap is even greater for gender diverse populations. In most cases, research does not account for gender-diverse identities, and presents the data in a binary of “male” and “female”.
When we are referencing a study, whether it is on social media, our website, or any of the conversations we engage in, we are constrained by the details of that study.
We will always present evidence-based facts as accurately as possible to represent the study that we are referencing. This means that sometimes, we are restricted to referring to “women” when we reference a study, even though we recognize that this only refers to sex, and not gender. We choose our language in these instances on a case-by-case basis that honors the factual information of the study, while respecting and acknowledging that the statistics don’t tell the whole story.
Prioritizing Inclusion
Some people may dislike or disagree with the words we choose to use. There are people who argue that inclusive language leads to an erasure of cisgender women and their experiences. This is not our belief. We recognize the unique experiences and strengths of everyone in our community. We stand by our transgender and non-binary community members. We support their right to accessible and affirming healthcare. The inclusivity of one person is not the erasure of another, but rather a strengthening of an entire community.
We cannot give the best care to anyone if we are not thinking about everyone. By treating the people we serve as a sum of their physical parts — rather than the complexity of their whole identity — we do a disservice to all, and the standard of care will never improve.
We also invite cis-men in partnerships with pregnant-capable people to join our community as individuals whose family planning efforts are supported by .
Treating as a women’s issue affects our ability to care for those who need that aren’t women, and takes them out of a conversation that they should be a part of. Everyone should feel safe and understood when seeking medical care. If we center our conversations about around women, we do everyone a disservice.
Our Commitment to You
As language evolves, so will we. Sometimes adyn may mess up, but we are building a community where it is safe to hold each other accountable for our mistakes and learn from them.
If you want to talk with us about language, inclusivity, affirming care, or how we can best serve our community, please email us at [email protected]. We invite conversations and learning opportunities. You know you best, and we want to get to know you better.
At adyn, we’re committed to:
- Celebrating and supporting gender diversity in our team and our community
- Using your pronouns
- Understanding how your biological age impacts your health decisions
- Working with partners within the LGBTQ+ community and engaging in continual conversation and learning in order to grow and serve our community better
- Hiring culturally-competent care providers so that none of our LGBTQ+ patients will have to educate their doctor on their own care
- Believing the experiences of our LGBTQ+ community members, and honoring the way they ask to be treated.
That all starts with the words we use.
Additional Resources
- The Gender Unicorn [Trans Student Educational Resources]
- A Guide to Gender Identity Terms [NPR]
- Trans + Gender Identity [The Trevor Project]
- Treating as a Women’s Disease Hurts Patients of All Genders [Vice]