We admire the iconic London underground as much as anyone, but “Mind the Gap” has a different meaning for us at adyn. The gap we’re “minding” – and calling attention to – is the medical knowledge gap, specifically the medical gender and race research gaps. These knowledge disparities have profound and devastating impacts on available diagnostics, treatment, and care for non-male, non-white populations. Our mission at adyn is to make scientific discovery more inclusive, which means not only shining a light on those gaps, but actually closing them.
Medical gender research gaps exist because the vast majority of biological literature is based on single-sex studies of males. From 1977-1993 women were essentially banned from participating in clinical trials; it wasn’t until 1993 that women were required to be included. While this ban was initially designed to protect women (and likely even more highly motivated by protecting fetuses), it led to widespread issues with adverse events and doses of drugs in women. In fact, between 1997 and 2001 ten prescription drugs were withdrawn from the US market with 8 of the 10 withdrawn because of more adverse events in women.
The long-lasting result of this historical bias towards studying male biology is, unsurprisingly, a lesser understanding of the female body.
As the Associate Director for Research on Women’s Health and Director of the Office of Research on Women’s Health at the N.I.H., Dr. Janine Austin Clayton put it, “We literally know less about every aspect of female biology compared to male biology”.
Similarly, human genetic research has been heavily biased in favor of individuals of European ancestry, despite the fact that worldwide, Europeans and their descendants make up just 12 percent of the .
Biased research leads to biased genetic datasets, resulting in accurate diagnosis of conditions and appropriate treatment protocols in people of European ancestry, but not necessarily for people from other racial backgrounds. Luckily, many discoveries made in one apply to other populations (we even learn things in mice that advance treatments in humans!). However, failure to make research inclusive of diverse populations means that we understand less than we could about human biology and disease and have disproportionately identified genetic risk and pharmacogenetic markers for individuals of European ancestry.
So how did we get here?
Gender Research Gaps
Our world is organized by disparities. For example, pay gaps, poverty, housing, education, the list goes on and on…but these disparities are not inherent; they are created through larger systems. As a female-founded company, we are well-acquainted with what gender inequality looks like.
- In the workplace, women earn less than their male counterparts of the same race and ethnicity at every level of educational attainment.
- In 2020 only 28% of U.S. startups had at least one female founding member
- Women age 19-44 incurred 80% higher health expenses compared to men of the same age, and yet only 3.3% of digital health funding went towards women’s health ventures.
Unequal support for female-led innovations is what leads to the advancement of products like single-use pink gloves for removing tampons instead of early detection, diagnostics, or improved treatments for the 97 health conditions that solely, disproportionately, or differently affect people assigned female at birth.
Like what you’re reading? Get the latest straight to your inbox 💌
Why research must be more gender-inclusive
Gender inequity is evident beyond the boardroom; it is in our labs, our exam rooms, and our current standard of medical care.
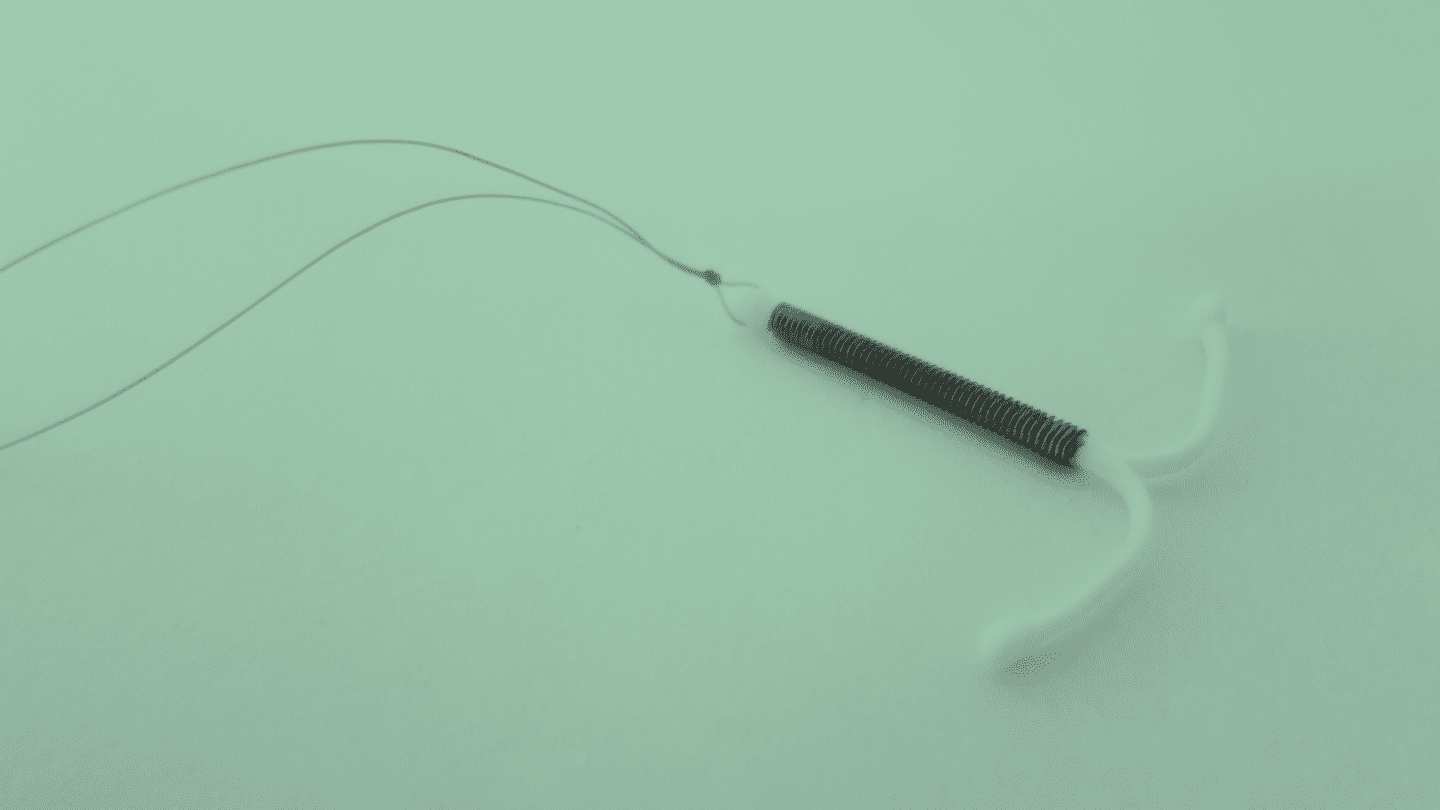
Around 60% of all women of reproductive age are currently using a contraceptive method. In the US, the average family wants to have two or three kids. Based on the average reproductive age range (15-49), this means that a woman would need to use for nearly 30 years (or avoid sex).
The pill has been on the market in the US since 1960 and has seen very little technological innovation. The numbers say it all: pharmaceutical companies typically spend ~20% of their revenue on research and development for new products but for they’ve spent only 2%. From 2017-2020 there were only 23 industry-funded clinical trials for contraceptives, but hundreds for both cardiovascular drugs and treatments relating to eye disorders.
Real talk: this means that for 61 years, people have been suffering from side effects with no ability to discern what a better option might be without going through trial-and-error. With nearly 200 different methods, that trial-and-error can be extensive, leaving too many contraceptive users suffering from side effects.
Despite the being well-established, medical research has not materially improved and in some cases, has become more troublesome. In pharmacology, the proportion of studies that accounted for sex in their data analysis has trended downward, from 33% in 2009 to 29% in 2019, even though the number of studies that included female research subjects grew by 21% over that 10-year timeline.
People born with make up ~50% of the . Research should reflect the .
Race Research Gaps
While research gaps place women of all races at a disadvantage, race gaps create further inequities for people of color.
People of color experience higher rates of illness and death than their white counterparts across the United States. In fact, when we look at all causes of death in people under 65, Black people have 40% higher death rates than white people.
Despite these staggering statistics, the distribution of medical research time, effort, and dollars isn’t correlated with the burden of disease. Black women are 3 times more likely to have than their white counterparts. According to endocrinologist Dr. Erica Marsh, “If men had … we would be much farther along in our understanding of them, and I think it’s largely [because ] disproportionately impact African American women, but really, impact all women” (Source).
The unequal distribution of medical research is glaringly apparent in genome-wide association studies (which look for genetic changes associated with disease). As of 2018, these studies were comprised of 78% individuals of European descent while only 10% were Asian, 2% African, 1% Hispanic, and less than 1% for all other groups.
The detrimental impact of leaving groups of people out of research cannot be overstated. Without ethnic diversity in research, our ability to understand the genetic architecture of human disease is impaired. Once again, these disparities are not inherent or natural. They are systematic: a result of racism and a history of prioritizing white people over the global majority – often excluding people of non-European descent in research.
Furthermore, when scientists have conducted research in less homogeneous groups (aka not just white males) we have made critical discoveries. For example, genetic mutations (in the PCSK9 ) identified in a woman of African descent helped scientists understand how cholesterol is regulated in all humans.
It’s important to know that there is a dark history of medical experimentation on people of color in unethical ways. A good example is how poor Puerto Rican women were targeted as test subjects for the development of . A more infamous example is the use of cervical cancer cells taken from Henrietta Lacks in 1951; her cells were nicknamed “HeLa” cells and have been used to research cancer and many other biological questions (even helping in the development of the Covid-19 vaccines) but these cells were taken without her consent.
Continuing to ignore race and gender medical gaps in research leads to structural biases in healthcare.
How racial gaps in research affect care
Individuals with intersecting identities (race, sexuality, gender identity, disability, etc) systemically experience compounding biases and inequities in everything from interpersonal interactions with providers, to access to care and overall health outcomes. In healthcare, it’s not just implicit bias in providers but also long-held false beliefs around biological differences between races.
Racism in healthcare is well documented and at large. From conception to pregnancy to pain (and beyond) — non-white patients face discrimination that threatens their lives:
- A study of 326 African American women showed that 67% reported race-based discrimination when obtaining family planning services. This discrimination was especially prevalent among women with a stronger Black identity, younger age, and lower-income.
- Around 700 women die each year in the U.S. from pregnancy-related complications; 3 out of 5 of these instances of maternal mortality could have been prevented. Black women are also 3 times more likely to die from pregnancy-related complications than white women. (If you haven’t read Serena Williams’ harrowing story about gaslighting by providers during postpartum complications, we highly recommend it.)
- In 2016, half of 418 surveyed white medical trainees held beliefs such as, “Black people have thicker skin” or that “Black people have less sensitive nerve endings than white people”. The result of these beliefs? Black and Latina patients are 22% less likely to receive pain medications than white patients.
Closing the gap
So how do we do it? To close genetic research gaps, we need to do four things:
- Analyze biological data from diverse populations
- Collect relevant medical history and treatment information
- Do this on a massive scale
- Establish trust and provide value in the form of medically actionable results to accomplish steps 1-3
But the gap is bigger than just data sets and genetics. Closing the gap is foundational to adyn– it is our founder’s story and it is our mission. This is our platform to talk about the taboo, but we want our money to be where our mouth is and challenge the current standards.
We close the pay gap through our hiring and employment practices. We hire culturally competent, compassionate telemedicine providers to serve our customers, and we work with partners with similar values. Our goals are geared toward closing more gaps: we want our product to be accessible to all people seeking highly effective , inclusive of data sets to refine and improve our recommendations, and expandable into new areas that can service people’s , fertility, and trans health needs. We are here to improve the standard of care for more people. We are here to mind – and close – the gap.