Maybe you have heard of an ectopic pregnancy but don’t quite know what it is (besides not a good thing). Maybe you are going through one right now or a good friend is– if that’s the case, we’re sorry it is happening to you. It can be a trying physical and emotional experience. Read on for the facts about ectopic pregnancies, healthcare options for treating them and addressing your fertility afterwards.
What is an ectopic pregnancy?
An ectopic pregnancy is when a fertilized egg implants outside of the main uterine cavity (where it is supposed to implant). An ectopic pregnancy is not viable.1 Most importantly, an ectopic pregnancy can be life threatening to the pregnant individual and should be treated by a physician immediately.2
While they are super scary and traumatic, please keep in mind that they happen rarely. Their frequency is estimated at 1 in 100 for people undergoing fertility treatments and 1 in 30,000 for people with spontaneous pregnancies.3 Other estimates suggest rates of 1-2% in the general .4-5 No matter how you were or were not trying to get pregnant, an ectopic pregnancy is not a fun experience and also one not commonly talked about. But, because of their possible severity, it is important to understand a bit more about them.
How do you recognize an ectopic pregnancy?
Initially, it can be difficult to know if a patient is experiencing an ectopic pregnancy because symptoms can be similar to a new healthy pregnancy: a missed period, tender breasts, nausea.1 Well, that’s pretty frustrating, huh? However, symptoms become more noticeable and distinct as an ectopic pregnancy continues and can include vaginal bleeding, cramping or pelvic pain, and lower back pain. If you have more severe symptoms such as shoulder pain, sudden and/or severe pelvic pain, weakness, extreme lightheadedness or dizziness and/or fainting, these could indicate a ruptured fallopian tube and you should immediately go to the emergency room.1-2 The safe course of action when experiencing any of these severe symptoms when it is possible that a patient is pregnant is to seek medical attention.
What are the dangers of an ectopic pregnancy?
The scary part of an ectopic pregnancy–and why it is great you are reading this to be informed–is the potential dangers it poses to someone experiencing one. If an ectopic pregnancy grows, it can cause the fallopian tube to burst or rupture. This can cause severe internal bleeding and is a life threatening situation. Ectopic pregnancies can also become life threatening situations if implantation occurs in rare locations such as the abdomen.6 Obviously, no one wants this situation to happen! If you or someone you know thinks they could be pregnant and are experiencing symptoms consistent with an ectopic pregnancy, seek immediate treatment by a physician. Experiencing an ectopic pregnancy is undoubtedly frightening and harrowing both physically and mentally. Please be kind to yourself if this is something you’ve gone through.
What causes ectopic pregnancies?
Frustratingly, there are no known direct causes of ectopic pregnancies.
Are there risk factors associated with them?
While there are no known direct causes of ectopic pregnancies, there are identified risk factors that elevate a patient’s chance of having one. Remember, having one or more of these factors does not mean you will have an ectopic pregnancy. The risk factors identified by the American College of Obstetricians and Gynecologists include:2
- age (being over 35)
- a previous ectopic pregnancy
- prior fallopian tube, abdominal or pelvic surgery
- certain sexually transmitted infections
- diagnosis of or pelvic inflammatory disease
- undergoing in vitro fertilization treatments
- smoking
- diagnosis of
If you know you have these risk factors and think you could be experiencing an ectopic pregnancy, please reach out to your healthcare provider immediately. When we read deeper into the science behind these risk factors, we found a few more details to share about some of them.
Sexually Transmitted Infections (STIs)
First, STIs – specifically chlamydia. When assessed in nearly 12,000 patients, Chlamydia trachomatis infections were associated with an approximately 3-fold increased rate of ectopic pregnancies.7 In general, having a Chlamydia trachomatis infection is associated with multiple negative pregnancy and fertility outcomes. The risk of ectopic pregnancies was stronger with Chlamydia trachomatis infection in low-middle vs. high income countries.8
In Vitro Fertilization (IVF)
Second, in vitro fertilization (IVF). For patients undergoing IVF or other assisted reproductive technologies, a pregnancy can be everything they hope for, sometimes for years. So, seeing an elevated risk of an ectopic pregnancy can be yet another scary, sad, hard part of getting/being/staying pregnant for these people. However, in one 10-year longitudinal study of 7,352 pregnancies, the of ectopic pregnancy was similar in patients undergoing assisted reproductive technologies to the in the general .9 Yet, the authors noted that many of the pre-existing risk factors identified for ectopic pregnancies are often found at higher rates within the infertile .9
Birth Control
Third, . Because we are all about here at adyn, it is worth noting that ectopic pregnancies have (rarely) been seen in people using .10-11 When compared across many options, the risk of ectopic pregnancy was very similar, and incredibly low, for all forms.11 Interestingly, two studies found that low dose IUDs had slightly higher rates of ectopic pregnancies. So, if someone is already at an elevated risk for ectopic pregnancy, there is some evidence to suggest that an option other than low dose IUD might be their preferred contraceptive method.10-11 This would be a great conversation starter for your next discussion with a healthcare provider.
Is adyn right for you? Take the quiz.
What are your healthcare treatment options during an ectopic pregnancy?
Thankfully, although ectopic pregnancies can be scary and dangerous, doctors have a number of tools available today that can help in diagnosing and treating patients with (probable) ectopic pregnancies.
For diagnosis, a doctor often uses a combination of patient history (last menstrual period date, sexual activity), an ultrasound and surrounding areas, and a blood sample to diagnose a possible ectopic pregnancy. Sometimes, the lack of detection of an egg sac in the combined with other factors is enough for physicians to suspect an ectopic pregnancy.
Like what you’re reading? Get the latest straight to your inbox 💌
There are two major routes of treatment for an ectopic pregnancy: medication and surgery. Your healthcare provider will discuss the risks and expectations with either of these courses of action. Here at adyn, we believe you should always advocate for yourself and ask questions until you are satisfied with the explanation and your understanding.
For medications, the most often used is methotrexate. Methotrexate is given as a shot and can be given in either one dose or two doses, if one alone is not sufficient. A medical professional will take into account a number of factors before deciding if methotrexate is the right course of action.2
Methotrexate can be used with or without mifepristone. The data and opinions on whether to use them together or not seem mixed and more clinical trials are needed.12-14 Either of these drugs will cause the developing ectopic pregnancy to stop growing, after which the patient may reabsorb the tissue or experience bleeding, which can resemble a period or miscarriage.
If medication is not possible, an emergency laparoscopic surgery (which requires general anesthesia) will be performed. The goal is to remove the unviable pregnancy and/or the tissue around it, depending on the patient’s specific situation. This can include removing a fallopian tube, or part of it, if the ectopic pregnancy is located there. (Spoiler alert– even if part of a fallopian tube must be removed, a patient could still become pregnant– see below.)
Besides these treatments for the physical condition, experiencing an ectopic pregnancy can be a heavy weight emotionally too. Although not part of standard recommendations, seeking mental and emotional support after an ectopic pregnancy could be extremely helpful for patient coping.
Can you get pregnant after an ectopic pregnancy?
In short, yes, it is very likely that you can become pregnant after an ectopic pregnancy. There are a few important notes to keep in mind once you’ve gone through an ectopic pregnancy, whether you want to become pregnant or not.
First off, methotrexate is a potent immunosuppressive drug that is lethal to all fetuses it has been tested against (this has been known for nearly 50 years).15 While it acts quickly, it can also take some time for your body to fully clear the drug and normalize its effects. So, if you were treated with methotrexate and you would like to become pregnant, some healthcare providers suggest waiting a number of months before trying to conceive again. There is also data that say there is no increase in fetal malformations if conceived within six months of taking methotrexate. More data is needed to make better conclusions, but the safe play, especially with what is at stake, is to wait at least three months.16
Second, it is important to remember that a previous ectopic pregnancy puts you at higher risk for another one. According to both the Mayo Clinic and a 2001 paper that followed 383 women over 3 years, the recurrence rate is ~10%.17,3 Be sure you are aware of the symptoms if you are in a position where you could become pregnant again after having an ectopic pregnancy.
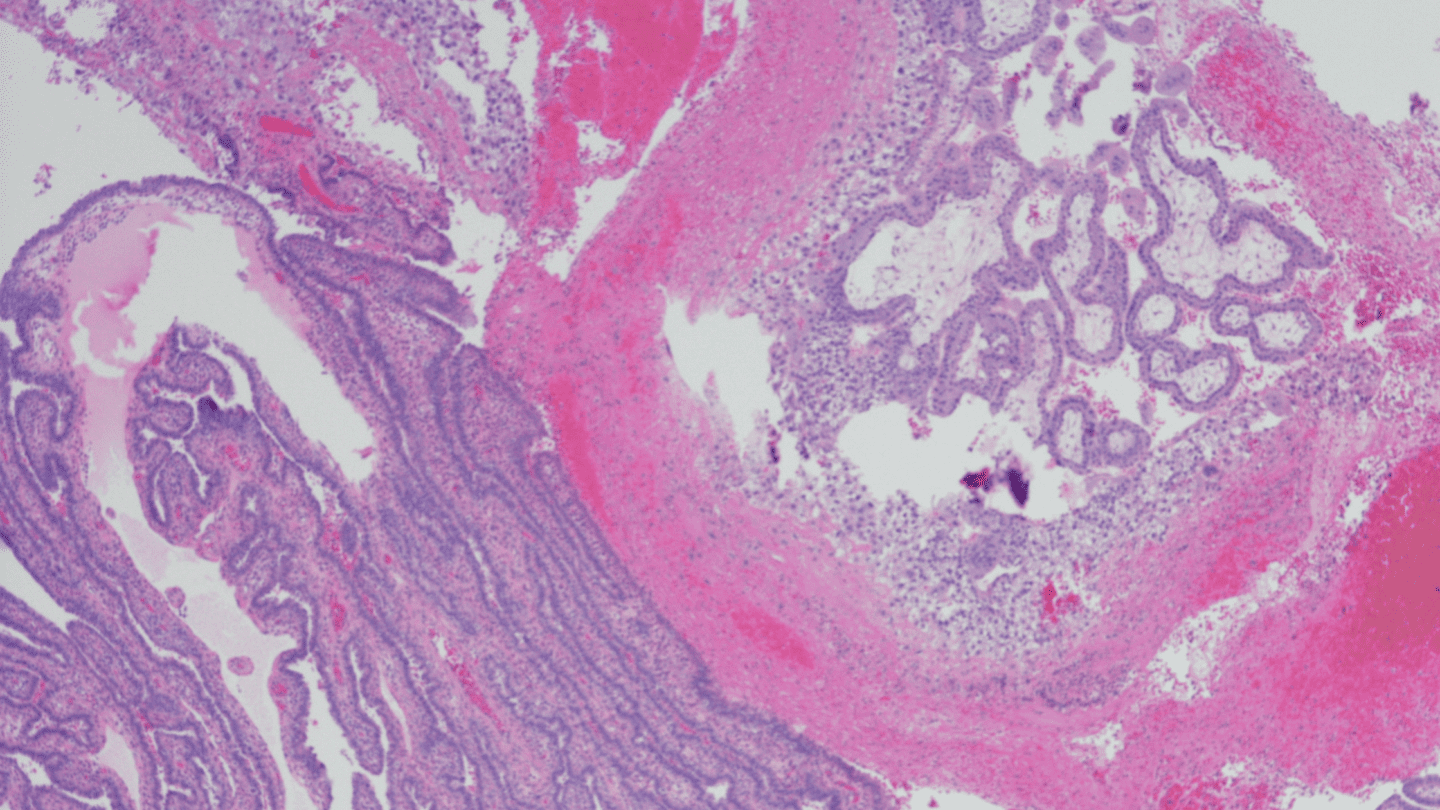
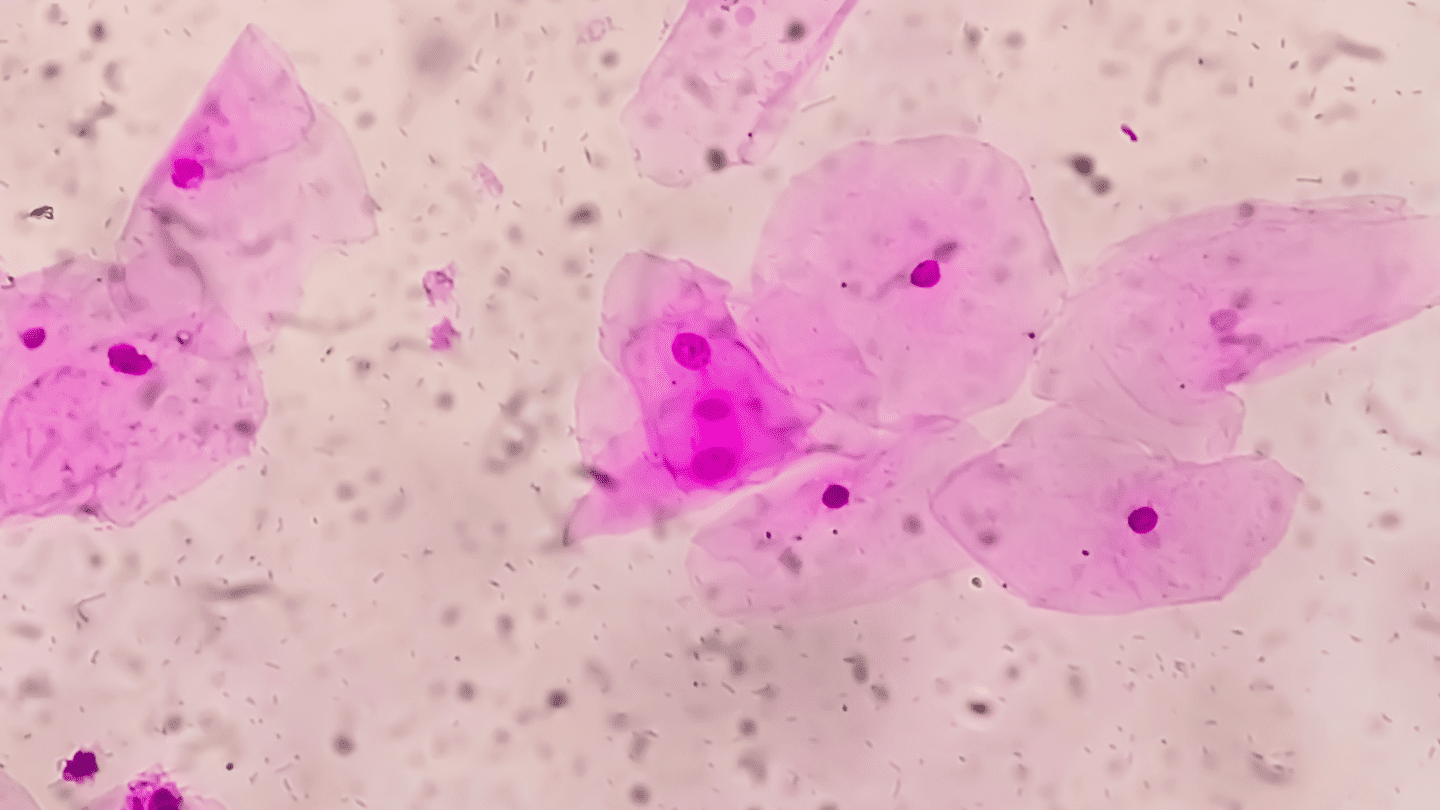
Micrograph of an ectopic pregnancy. Credit: OGphoto from Getty Images Signature
The good news is that you can also become pregnant regardless of the type of treatment you received for an ectopic pregnancy – even if a fallopian tube was removed.3,18 If surgery must be performed and tissue is removed, that can increase the chance of challenges in becoming pregnant in the future, but doesn’t rule out the possibility.
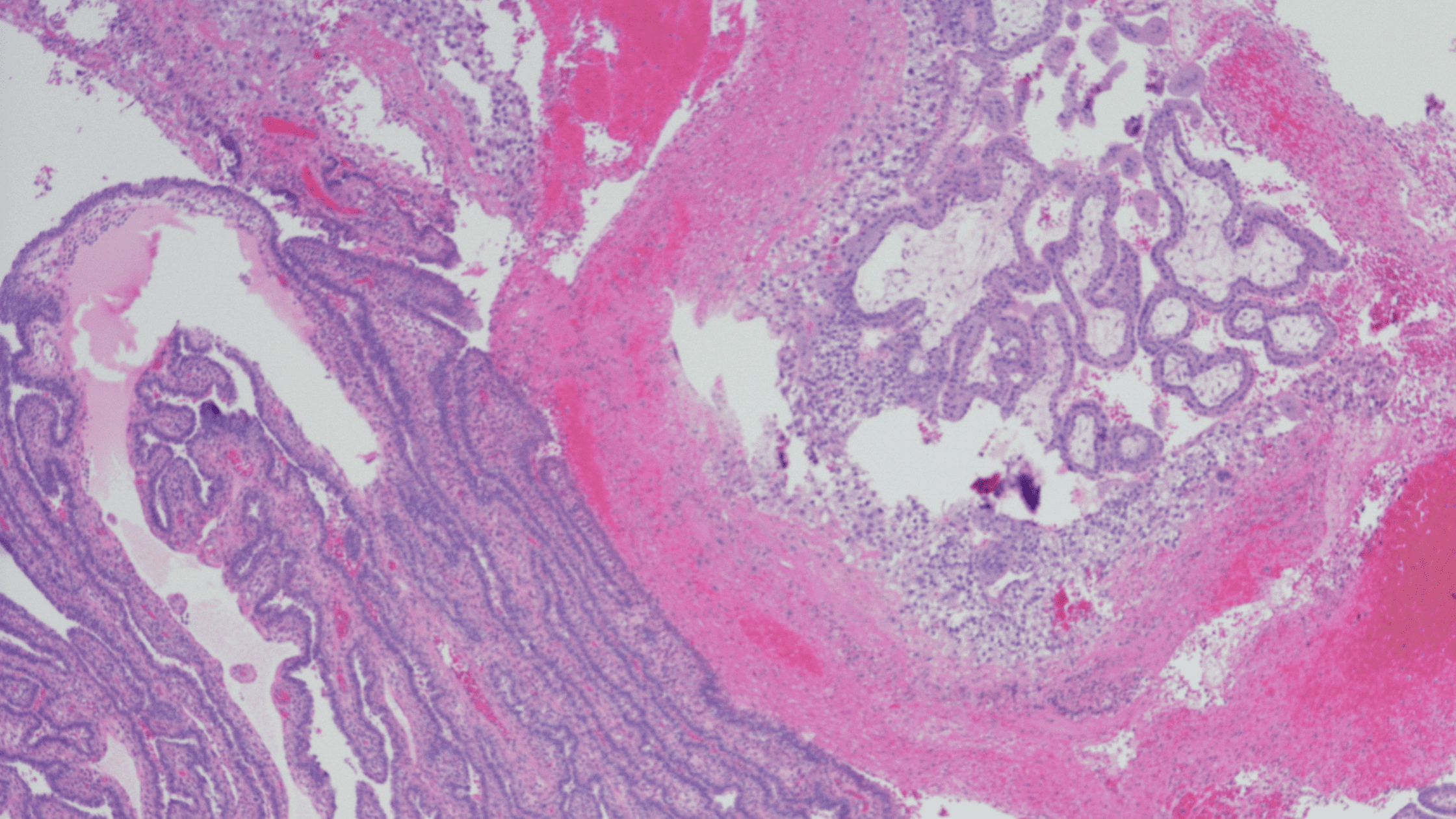
Are there different types of ectopic pregnancies?
Yes. One way that ectopic pregnancies can be categorized is by where the egg implants. Ninety percent (90%) of ectopic pregnancies implant in the fallopian tube,2 meaning, they just don’t travel quite far enough before implanting. Other rare locations for an ectopic pregnancy include in the abdominal cavity (primarily in pouches around the )6 or in the cervix or .19
Very rarely (only 19 cases total reported as of 2002),20 ectopic pregnancies can occur if the egg implants in the muscle or fibrous tissue of a cesarean scar.21 Importantly, this is an extremely rare occurrence, but one that obstetricians are concerned with given the increased number of pregnancies ending with cesarean procedures and diagnosis capabilities that are increasingly better at identifying ectopic pregnancies.21 If a healthcare provider is suspicious of an ectopic pregnancy, all of these possible locations will be considered while choosing the best course of action to keep you safe.
Conclusion
The bottom line: An ectopic pregnancy can be a life threatening situation. If you are ever concerned that you or someone you know could be having an ectopic pregnancy, please seek immediate medical care.
Physically, recovery from an ectopic pregnancy can vary depending on each patient’s situation. Emotionally, experiencing an ectopic pregnancy can also feel so different to different people: traumatic, scary, unexpected, frustrating, heartbreaking. Consulting a therapist or counselor can be helpful for those who go through an ectopic pregnancy. Take care of yourself and seek support during healing and coping with the event both physically and mentally.
If you are sexually active, use until you feel like you are ready to become pregnant. The Birth Control Test can help you find the right highly-effective method for your unique body.
-
- Mayo Clinic Staff. “Ectopic Pregnancy.” MayoClinic.org. (2022 Mar 12: Last accessed 2023 Feb).
- “Ectopic pregnancy.” ACOG.org. (2022 Jul: Last accessed 2023 Feb).
- Khalife, Tarek. “Ectopic pregnancy: Signs, treatment and future fertility.” MayoClinicHealthSystem.org. (2022 Feb 08: Last accessed 2023 Feb).
- Raine-Bennett, Tina, et al. “Disparities in the Incidence of Ectopic Pregnancy in a Large Health Care System in California, 2010− 2019.” The Permanente Journal 26.3 (2022): 61.
- Centers for Disease Control and Prevention. “Ectopic pregnancy–United States, 1990-1992.” Morbidity and Mortality Weekly Report 44.3 (1995): 46-48.
- Poole, Aaron, David Haas, and Everett F. Magann. “Early abdominal ectopic pregnancies: A systematic review of the literature.” Gynecologic and Obstetric Investigation 74.4 (2012): 249-260.
- Xia, Qingchang, et al. “Relation of Chlamydia trachomatis infections to ectopic pregnancy: A meta-analysis and systematic review.” Medicine 99.1 (2020).
- Tang, Weiming, et al. “Pregnancy and fertility-related adverse outcomes associated with Chlamydia trachomatis infection: A global systematic review and meta-analysis.” Sexually Transmitted Infections 96.5 (2020): 322-329.
- Cirillo, Federico, et al. “Ectopic pregnancy risk factors in infertile patients: A 10-year single center experience.” Scientific Reports 12.1 (2022): 20473.
- Elgemark, Karin, et al. “The 13.5-mg, 19.5-mg, and 52-mg levonorgestrel-releasing intrauterine systems and risk of ectopic pregnancy.” Obstetrics & Gynecology 140.2 (2022): 227-233.
- Kopp-Kallner, Helena, et al. “Method of hormonal contraception and protective effects against ectopic pregnancy.” Obstetrics & Gynecology 139.5 (2022): 764.
- Gazvani, M. R., et al. “Mifepristone in combination with methotrexate for the medical treatment of tubal pregnancy: A randomized, controlled trial.” Human Reproduction 13.7 (1998): 1987-1990.
- Su, Qiling, et al. “The efficacy of mifepristone combined with methotrexate for the treatment of ectopic pregnancy: A systematic review and meta-analysis.” Annals of Medicine 54.1 (2022): 3268-3284.
- Xiao, Chao, et al. “Non-surgical management of tubal ectopic pregnancy: a systematic review and meta-analysis.” Medicine 100.50 (2021).
- Jordan, Robert L., James G. Wilson, and Herbert J. Schumacher. “Embryotoxicity of the folate antagonist methotrexate in rats and rabbits.” Teratology 15.1 (1977): 73-79.
- Hackmon, Rinat, Sachi Sakaguchi, and Gideon Koren. “Effect of methotrexate treatment of ectopic pregnancy on subsequent pregnancy.” Canadian Family Physician 57.1 (2011): 37-39.
- Ego, Anne, et al. “Survival analysis of fertility after ectopic pregnancy.” Fertility and Sterility 75.3 (2001): 560-566.
- Baggio, Silvia, et al. “Fertility and reproductive outcome after tubal ectopic pregnancy: comparison among methotrexate, surgery and expectant management.” Archives of Gynecology and Obstetrics 303 (2021): 259-268.
- Tay, Jackie I., Judith Moore, and James J. Walker. “Regular review-Ectopic pregnancy.” British Medical Journal 320.7239 (2000): 916-919.
- Fylstra, Donald L. “Ectopic pregnancy within a cesarean scar: A review.” Obstetrical & Gynecological Survey 57.8 (2002): 537-543.
- Pędraszewski, Piotr, et al. “Cesarean scar pregnancy–a new challenge for obstetricians.” Journal of Ultrasonography 18.72 (2018): 56-62.