If you have migraines, you want relief — and you’re definitely not interested in anything that might make them worse. And if you don’t have migraines, you’re certainly not looking to start! That’s why it’s important to know the risks — and benefits — that might be associated with taking when it comes to migraines.
The question of whether helps or hurts migraines is a tricky one, since the short answer is: it depends. For some people, the hormones in some methods can make their migraines better, but others see the opposite effect. And sometimes, can even cause migraines in people who never had them before. Different bodies react differently, so you’ll need to find what works best for you.
What are migraines?
Migraines are more than just “bad headaches.” They’re a complicated, recurring condition that comes with many symptoms, including throbbing and pulsing pain in the head, dizziness, fatigue, nausea, and to light, sound, or smells.1
Regular headaches are just head pain from a specific cause, like dehydration or illness. Migraines, on the other hand, have different triggers for different people, but their root causes are not well understood. Scientists say they still don’t fully understand what causes migraines, or why they can vary so much from one person to another. But they think that some combination of a person’s genetics, environment, hormones, and even allergies can all play a role.
How do hormones affect migraines?
Migraines are three times more common in women than in men.2 This is because of the way fluctuations in — like the ones that happen during a person with a ’s monthly cycle — can influence your brain. Specifically, the drop in can revv up cells and blood vessels in a way that causes pain, nausea, and more.
Migraines are three times more common in women than in men.
Around 60-70 percent of women who have migraines say they notice a connection between migraine attacks and their periods.3 Experts call this “menstrual migraine,” and it’s typically experienced as a migraine right before and/or during a period, caused by the drop in that occurs at that point in the cycle.3
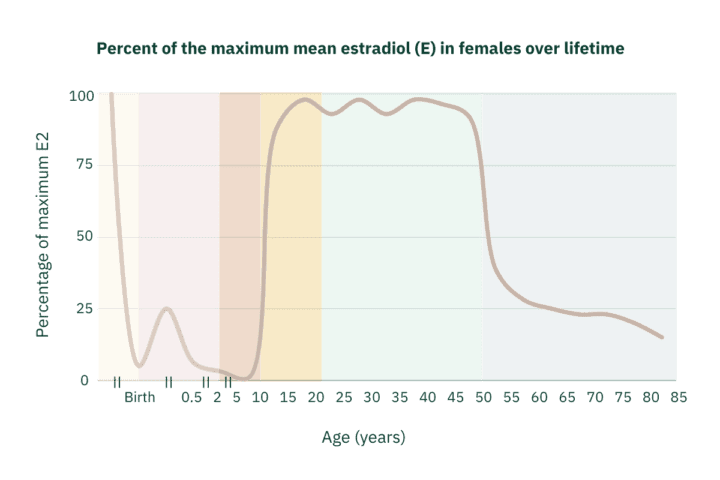
Adapted from: Figure 1 in Ober, Carole, Dagan A. Loisel, and Yoav Gilad. “Sex-specific genetic architecture of human disease.” Nature Reviews Genetics 9.12 (2008): 911-922.
For many people with a , their migraines track with their life stage, starting during puberty, and waning during . Some migraineurs report that their migraines went away while they were pregnant, while some people without migraines say they started to have them during their first trimester.3
Researchers can even see an interaction between migraines and biological sex in the brain. When scientists looked at MRIs of people of different sexes, with and without migraines, the anatomical differences they saw in the brains of people who had both migraines and uteruses were stark. The brains of females with migraines were different from both the brains of females without migraines and from the brains of males with migraines,5 showing that something complex is going on in these brains.
Like what you’re reading? Get the latest straight to your inbox 💌
Why can help migraines…sometimes
Many people find that using hormonal contraceptives helps their migraines. That’s because the drugs regulate levels across the cycle, resulting in less dramatic fluctuations in the and fewer migraines. It’s the same reason birth control helps PMS and PMDD symptoms for some people.
A number of studies have analyzed how many people see improvements to their migraines on hormonal birth control, but they don’t all agree. For example, one review looking at many studies found that anywhere from 3-35% of people reported improvements to their migraines, 18-50% reported worsened migraines, and 39-65% of people saw no change.2
In general, people who do see improvements tend to be using extended-cycle forms of hormonal like pills with fewer inactive/ days.6 That’s because these forms keep levels the steadiest over the course of the cycle.
That said, everyone is different. Some people have actually reported that they started having migraines as a side effect from their .7 If that happens to you, or your existing migraines have gotten worse on , talk to your provider about switching to a different method, like a progesterone-only option.7
Is adyn right for you? Take the quiz.
Migraine with aura
Some people have a unique form of migraines called migraine with aura. This “aura” is a set of sensory symptoms people experience right before the onset of their headache, like seeing spots or flashes of light, feeling tingling in their hands or face, or even trouble speaking.7
Migraine with aura is also correlated with a higher risk for blood clots and strokes. Estrogen-containing contraceptives also raise the risk for these things, so providers typically won’t prescribe them to people who have migraines with aura.8 Likewise, estrogen-containing could also be riskier for people with a family history of migraine with aura or blood clots, or who are smokers.
Why aren’t migraines studied more?
Migraines are a complex condition, but that’s not the only reason we know so little about them. When you compare funding to disease burden (how many people have a disease and how much it affects them), migraines are one of the most under-funded conditions out there.9-10 And like the rest of the top seven under-funded conditions, migraines affect predominantly people with uteruses.10 Think that’s a coincidence?
Despite the lack of attention from the medical and research communities, it’s encouraging to know at least some foundational work has been done to understand the estrogen-migraine connection. For example, there is indeed solid evidence that, at least for some people, finding the right can help reduce migraines.
If you have migraines and would like to take , be sure to bring up both to your doctor to make sure you’re choosing a option that’s best for you (and check out The Birth Control Test!). If you’re starting a new hormonal contraceptive, pay close attention to whether your migraines get better or worse — you may even want to take day by day notes so you can better assess the change. And if your triggers new migraines or makes existing migraines worse, don’t settle! Talk to your doctor about switching to another option.
-
- Penn Medicine.“Migraine vs. Headache: How to Tell the Difference.” PennMedicine.org (2019 Nov 01): Last accessed 2022 Apr 21.
- Sacco, Simona, et al. “Migraine in women: the role of hormones and their impact on vascular diseases.” The Journal of Headache and Pain 13.3 (2012): 177-189.
- Cleveland Clinic. “Menstrual Migraines (Hormone Headaches)” ClevelandClinic.org (2021 Mar 03): Last accessed 2022 Apr 21.
- Ober, Carole, Dagan A. Loisel, and Yoav Gilad. “Sex-specific genetic architecture of human disease.” Nature Reviews Genetics 9.12 (2008): 911-922.
- Chai, Nu Cindy, B. Lee Peterlin, and Anne H. Calhoun. “Migraine and estrogen.” Current Opinion in Neurology 27.3 (2014): 315.
- Mayo Clinic Staff. “Headaches and hormones: What’s the connection?” MayoClinic.org (2020 Dec 10): Last accessed 2022 Apr 21.
- Mayo Clinic Staff. “Migraine with aura.” MayoClinic.org (2021 Jul 2): Last accessed 2022 Apr 21.
- American Migraine Foundation. “Spotlight On: Oral Contraceptives and Migraine.” AmericanMigraineFoundation.org (2018 Jul 05): Last accessed 2022 Apr 21.
- Schwedt, Todd J., and Robert E. Shapiro. “Funding of research on headache disorders by the National Institutes of Health.” Headache: The Journal of Head and Face Pain 49.2 (2009): 162-169.
- Mirin, Arthur A. “Gender disparity in the funding of diseases by the US National Institutes of Health.” Journal of Women’s Health 30.7 (2021): 956-963.