Is my biological clock ticking? Many will mistakenly turn to tests to answer this question — but research shows that a count of your eggs doesn’t mean what you might think it means. Although tests are frequently marketed as female fertility tests, the evidence says otherwise: The number of eggs in your has nothing to do with your pregnancy success. People with low egg counts are no less likely to get pregnant as those with high egg counts. Egg quality, not egg quantity, is what matters, and that’s not something doctors can currently test.
Egg quality, not egg quantity, is what matters.
Sadly, many companies offer tests to everyone, hyping them as fertility tests. This type of marketing preys on women’s fears of aging and , inspiring some to rush their pregnancy, needlessly freeze their eggs, or consider other big decisions based on bad info. These tests are useful for some things, like determining if you’re a good candidate for egg-freezing or IVF – procedures where quantity actually matters for outcomes.
Here’s what the evidence says about tests, so you can make an informed decision about whether to take one – and what to think if you’ve gotten a report on your egg count.
How do tests work?
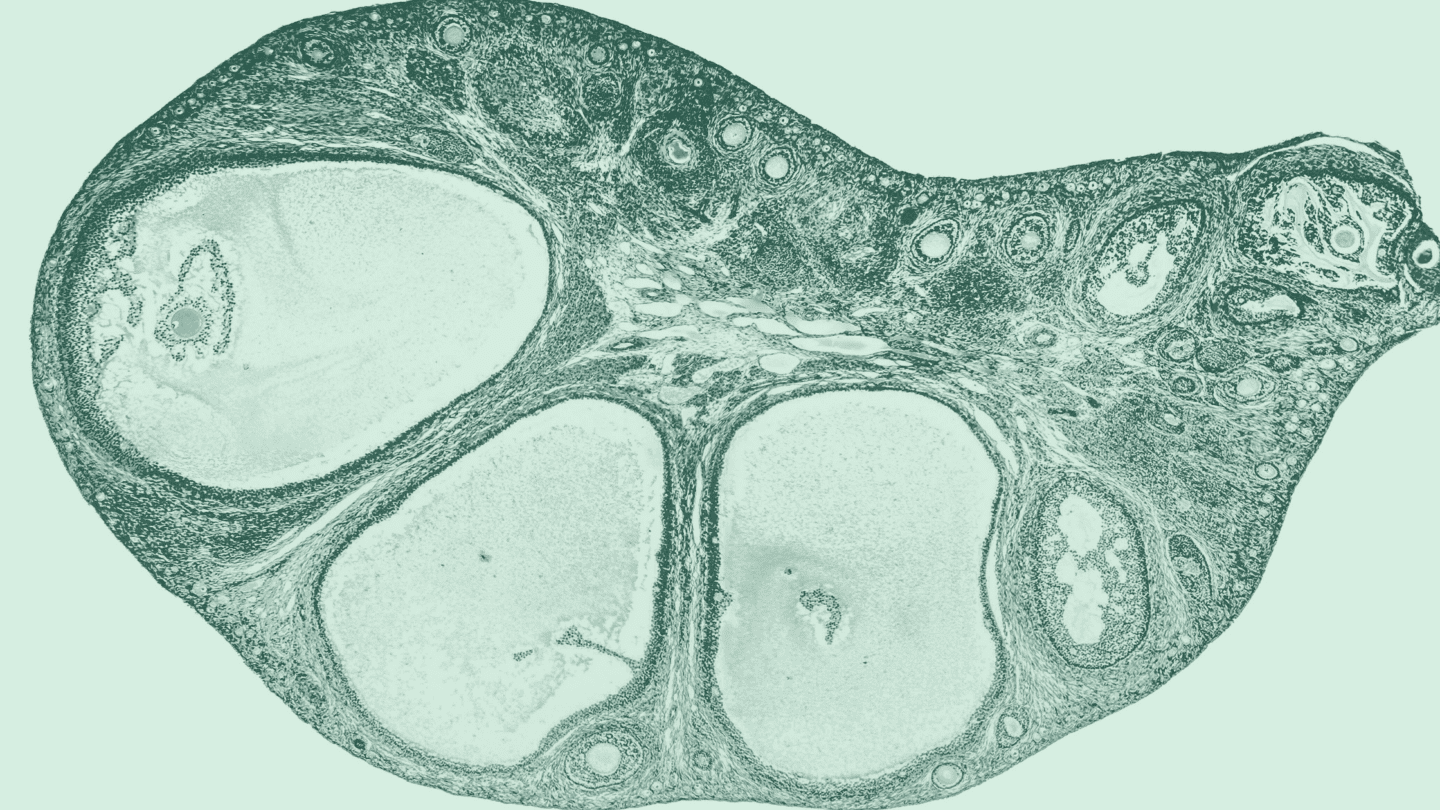
Ovarian reserve tests estimate the number of eggs present in your (your “ovarian reserve”). Most people going in for an test will encounter two or three tests.1 One is a blood test for (), a your reproductive cells produce that corresponds directly with the number of eggs you have.
The other is an ultrasound called an antral follicle count (AFC). Antral follicles are fluid-filled sacs that contain the eggs in your ; one egg is released from a follicle each menstrual cycle. On average, women in their 20s can have between 10 and 30 follicles, while women in their forties can have as few as four.2 Practitioners can count your follicles visually with a transvaginal ultrasound to approximate how many active follicles, which represents the number of potential eggs, you have left.
Like what you’re reading? Get the latest straight to your inbox 💌
Follicle-stimulating () tests are also common, though not as accurate as the previous two. This is made in your pituitary gland, and rises and falls with your cycle, peaking right before ovulation. Over a person’s life, levels rise as their egg counts fall.3
Why tests are misleading
Egg count declines steadily with age. But egg quality also declines with age4 — and that’s what actually matters when it comes to odds of a successful pregnancy.5 If an test indicates you have fewer eggs than the average woman your age, this does not mean your egg quality is lower too, nor does it mean your odds of pregnancy are any lower.
Imagine this: A 30-year-old woman takes a “fertility test” and learns her egg count is close to that of the average 45-year-old woman. She might conclude her reproductive system has aged faster than normal, that she’s running out of eggs — so if she wants a child she better get pregnant soon. But she’s been seriously misled: Her actual fertility is related to the quality of her eggs, not the quantity.
Unfortunately, there’s currently no test for measuring egg quality — the factor that actually matters for fertility. That’s why age is currently the best proxy for fertility that we have.
Is adyn right for you? Take the quiz.
What’s the best way to measure fertility?
The best way to check your fertility is to look at your age. Younger people have the greatest chance of getting pregnant, regardless of how many eggs they have. In fact, all people become gradually less fertile with age, especially after their mid-20’s, when fertility peaks.4,6-7 It’s a normal part of the aging process.
By the way: It’s a myth that female fertility magically drops off around age 35. Some say this idea comes from a 1997 study that’s commonly misinterpreted, while others have traced it back to 1700s France. Regardless of where the idea came from, there’s no fertility cliff at 35.8
Fertility is impacted by a number of factors that tend to be correlated with age, like overall health. For instance, eating well, maintaining a healthy weight, avoiding excessive stress, and not smoking have all been linked to better fertility. There’s also a number of other underlying health conditions that might affect fertility, like disorders related to the hypothalamus or pituitary glands,10 irregular cycles, ,11 and more.
Read more: Can Cause ?
Are tests ever useful?
Ovarian reserve tests are really only useful if you’re planning on starting IVF or freezing your eggs. Since the number of eggs you have is directly related to how many eggs can be harvested, an test will tell you if you’re a good candidate. For example, many fertility clinics recommend a person has at least four mature follicles before starting on treatments for IVF.
But if that’s not you, experts actually suggest that you don’t take an test unless you’ve been trying, unsuccessfully, to conceive for at least six months. Since tests don’t reflect your actual fertility, they might even mislead you into rushing, or putting off, trying to conceive.
The truth about fertility tests for women
In the end, it’s important to remember that people with low egg counts are no less likely to get pregnant as those with high egg counts. Your body releases one egg per cycle until , and that one egg is what has a shot at fertilization, implantation, and pregnancy – no matter how many others are waiting in the ranks.
Ovarian reserve tests that estimate the number of eggs are only useful in estimating a woman’s response to procedures requiring harvesting eggs, like IVF or egg freezing. It’s important to keep interpretations of results limited to that. In fact, experts recommend you don’t test your s just for the sake of knowing — it can ruin your peace of mind without providing helpful fertility info.
At adyn, we care about giving you information you can act on. Learn more about what we test and why.
-
- Tal, Reshef, and David B. Seifer. “Ovarian reserve testing: a user’s guide.” American Journal of Obstetrics and Gynecology 217.2 (2017): 129-140.
- Bozdag, Gurkan, et al. “Age related normogram for antral follicle count in general population and comparison with previous studies.” European Journal of Obstetrics & Gynecology and Reproductive Biology 206 (2016): 120-124.
- Jehan, Sarwat, and Sadiqa Syed. “Association of ovarian reserve with age, BMI and serum FSH level in subfertile women.” Journal Of Pakistan Medical Association 66.4 (2016): 409-413.
- Moghadam, Ali Reza Eftekhari, et al. “Oocyte quality and aging.” JBRA Assisted Reproduction 26.1 (2022): 105.
- Steiner, Anne Z., et al. “Association between biomarkers of ovarian reserve and infertility among older women of reproductive age.” JAMA 318.14 (2017): 1367-1376.
- Wood, James W. “Fecundity and natural fertility in humans.” Oxford Reviews of Reproductive Biology 11 (1989): 61-109.
- American College of Obstetricians and Gynecologists. “Having a Baby After Age 35: How Aging Affects Fertility and Pregnancy.” ACOG.org (2023 Feb).
- Mayo Clinic Staff. “Pregnancy after 35: Healthy pregnancies, healthy babies.” MayoClinic.org (2022 Jul 15).
- Sharma, Rakesh, et al. “Lifestyle factors and reproductive health: Taking control of your fertility.” Reproductive Biology and Endocrinology 11.1 (2013): 1-15.
- Mikhael, Sasha, Advaita Punjala-Patel, and Larisa Gavrilova-Jordan. “Hypothalamic-pituitary-ovarian axis disorders impacting female fertility.” Biomedicines 7.1 (2019): 5.
- Penzias, Alan, et al. “Fertility evaluation of infertile women: a committee opinion.” Fertility and Sterility 116.5 (2021): 1255-1265.