Nexplanon vs. IUDs: What’s the Difference?
There are a few different kinds of that go inside your body. But, as if picking wasn’t already confusing, only one of these actually gets called “the implant.” That would be Nexplanon, a small plastic rod that’s implanted into your arm and releases a sex into your bloodstream.1
Intrauterine devices, or IUDs, are also inserted into your body (but not “implanted,” if we want to get technical). IUDs also release a sex , and they prevent pregnancy in essentially the same way that Nexplanon does. The main difference is that IUDs are inserted into your , while the implant goes in your upper arm.2 Both the implant and IUDs are known as LARCs, or long-acting reversible contraceptives.
Both of these options for are highly effective, and they both last for years, meaning you don’t need to worry about remembering to take a pill every day or do any other kind of regular upkeep. There are a few specific side effects to both IUDs and the implant that you should think about though as you weigh the pros and cons. To make it easier for you, we’ve collected all of that info below.
Is adyn right for you? Take the quiz.
Differences between the implant and an IUD
The implant, which typically goes by the brand name Nexplanon, is a four-centimeter-long plastic rod that doctors insert into your arm. It contains a , which it releases slowly to prevent pregnancies.1
IUDs like Mirena, Kyleena, and Paragard are T-shaped devices that a doctor puts inside your .2 There are two kinds: hormonal IUDs and copper IUDs. The hormonal kind releases just like the implant, while the copper IUD changes the chemistry of your in a way that stops sperm from working (safely).3
The one major difference between the implant and IUDs is how and where they get inserted. The implant is placed in your upper arm using a custom-made tool.1 Your provider will numb your arm with a shot before the insertion, which is the only potentially painful part of the implantation process.4 Most people say it’s not a huge deal.
IUDs are put into your through your . The procedure is the same no matter the brand, and it only takes a few minutes. The top arms fold out once it’s in your to hold it in place, and there’s a small string that’s used to take it back out.

Benefits of the implant or an IUD
Both IUDs and the implant are more than 99% effective at stopping pregnancies.1-3 And all IUDs and the implant are considered safe for most people.1-3
For some users, the big advantage of both the implant and IUDs is that once they’re put in place, you can pretty much forget about them. They release hormones automatically, and you don’t need to do anything until years later when they need to be replaced.
Birth control isn’t the only reason to consider getting an IUD or the implant, either. also helps regulate periods, control heavy or irregular bleeding, and more.5 If you’re one of the many people thinking about using hormonal for reasons other than preventing pregnancy, an implant or IUD might be an easy option for you.
Like what you’re reading? Get the latest straight to your inbox 💌
How the Nexplanon implant works
The implant is a plastic rod that’s filled with 68 mg of etonogestrel, which is a . It’s sold under the brand name Nexplanon (an older version was called Implanon). The implant releases about 60 to 70 micrograms of its every day when it’s new, and it does so continuously.1
To implant it, a doctor or nurse will use a special tool to insert the rod just under the skin of your non-dominant upper arm. You should be able to feel it there, but it’s not bothersome for most people. The implant is good for three years, and then you’ll need to have it removed.1 At that point, it’s up to you whether you want to have a new one put in or not. You can also have the implant taken out whenever you want.
The the implant releases helps to stop ovulation and thickens your cervical mucus, which helps prevent pregnancies. And, like other options, the implant doesn’t affect your long-term fertility once you have it removed.6
How IUDs like Mirena work
Hormonal IUDs contain a called levonorgestrel, which they release slowly into your body. There are four brands currently approved by the FDA: Liletta,7 Kyleena,8 Mirena,2 and Skyla.9
An IUD looks like the letter T, with a long stem and two short arms at the top. The arms fold down during insertion, and once it’s in your , the top arms snap open to hold it in place. You don’t need to worry about you or your partner feeling it when you have sex, either — it’s located out of reach.2 The IUD has short strings that are reachable, though, which are there so you (and your doctor) can check to make sure everything stays in place.10 It’s unlikely your partner will feel them during sex.
Every hormonal IUD works in the same way, but different kinds will release slightly different amounts of their every day, and some need to be replaced sooner than others.8-9 At seven years, Mirena is the longest-lasting hormonal IUD right now.2
There’s also a non-hormonal IUD made out of copper, called Paragard. Instead of releasing s, the copper IUD interferes with how sperm swim, meaning they can’t make it all the way to fertilize an egg. It only needs to be replaced every ten years.3
How effective are implants and IUDs?
Both the implant and IUDs are highly effective , meaning they’re more than 99% effective at preventing pregnancy.
Studies of contraceptive users show that Nexplanon is 99.6% effective and Mirena is 99.3% effective.1-2 The copper IUD, Paragard, is also more than 99% effective.3 That’s more effective than almost any other method out there.11 IUDs and the implant have another benefit as well: they’re nearly impossible to misuse. Afterall, you can’t forget to take an IUD, or put an implant on. You’ll just need to get your device replaced on schedule — three years for the implant, and between three and ten years for IUDs, depending on the kind.
What are the side effects of Mirena and Nexplanon?
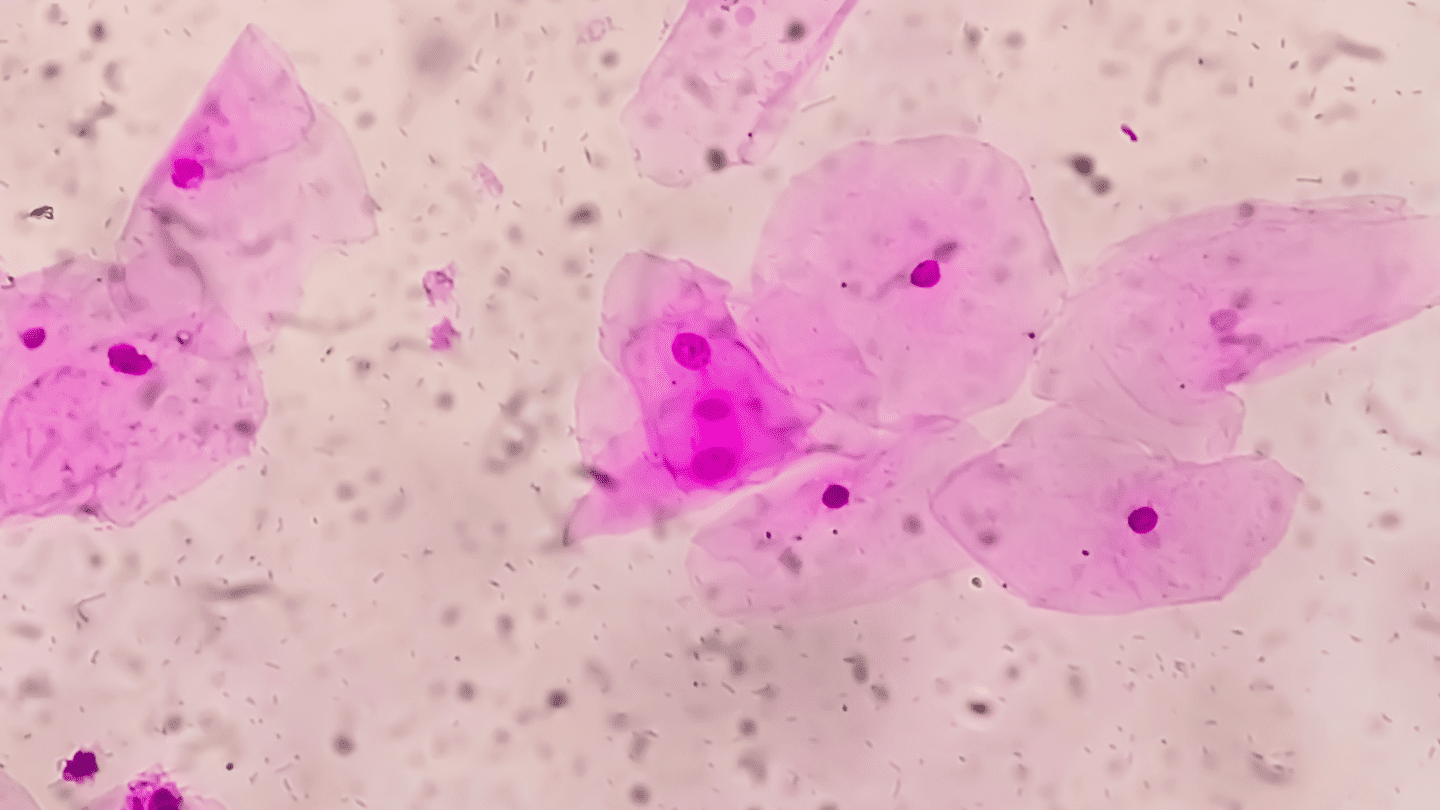
Both the implant and hormonal IUDs come with the same potential side effects as other kinds of . For example, 6-7% of people reported some pain during periods, and up to 25% said they experienced headaches. And other symptoms might include irregular bleeding or vaginitis (typically from a bacterial infection).1-2
Both the implant and hormonal IUDs come with the same potential side effects as other kinds of .
But don’t forget that there are positive side effects to hormonal birth control, too. Many people use it to help reduce painful or heavy periods, and it can help treat as well.4 What kind of good and bad side effects you might expect from any particular kind of depends a lot on your specific body. That means different IUDs releasing different amounts of their hormones every day might work better for some people and worse for others.
The copper IUD doesn’t cause the same kind of negative (or positive, for that matter) side effects that hormonal IUDs do. It can cause heavy bleeding and pain in some people, though that can improve over time.1-2
There is one note of caution around IUDs. While doctors typically say that getting them inserted or removed doesn’t hurt too badly, many people say otherwise. One study found that 78% of those who got an IUD put in rated the pain as “moderate to severe,” and many also felt nauseous or faint.13 Another study found that doctors consistently under-rated their patients’ pain. People getting an IUD inserted said their levels of pain were about twice as high as what their doctors thought.14
There’s no sign that getting an IUD put in will actually cause any kind of damage, except in very rare cases, like if the or other reproductive organs get infected.2 But the process can definitely be highly unpleasant, and you might not hear that going into the procedure. Still, for many people, getting an implant or IUD inserted is worth the peace of mind they get from not having to worry about taking . Ultimately, the decision rests with you.
Bottom Line
Both the implant and IUDs are highly effective , and they’re all good options for preventing pregnancies. Some hormonal options may work better for some people than others, and you should keep in mind that just because your body doesn’t respond well to one kind of hormonal birth control, that doesn’t mean it won’t respond better to another.
Implants and IUDs are good options for people who want they can forget about once it’s put in place. But, especially for IUDs, getting them put in and taken back out can be painful for some people. There are also different kinds of IUDs, so one kind might work better for your unique body than another.
Want better insights into your biology and what kind of is best for you? That’s what adyn is here for. Personalized insights give you the best information possible to make an informed decision.
Check out The Birth Control Test, the first test designed to prevent side effects.
-
- FDA. “NEXPLANON (etonogestrel implant).” (2018 Oct).
- FDA. “MIRENA (levonorgestrel-releasing intrauterine system).” (2020 Aug).
- FDA. “PARAGARD (intrauterine copper contraceptive).” (2019 Sep).
- Schrager, Sarina, et al. “Beyond birth control: noncontraceptive benefits of hormonal methods and their key role in the general medical care of women.” Journal of Women’s Health 29.7 (2020): 937-943.
- Planned Parenthood. “What happens when the birth control implant is inserted?” PlannedParenthood.org (N.D.): Last accessed 2022 Mar 14.
- Fraser, Ian S., and Edith Weisberg. “Fertility following discontinuation of different methods of fertility control.” Contraception 26.4 (1982): 389-415.
- FDA. “Liletta Levonorgestrel (LNG)-releasing Intrauterine System (IUS): Clinical Review.” (2019 Oct 18).
- FDA. “KYLEENA (levonorgestrel-releasing intrauterine system): Prescribing Information.” (2016 Sep).
- FDA. “SKYLA (levonorgestrel-releasing intrauterine system): Prescribing Information.” (2017 Mar).
- Planned Parenthood. “What’s an IUD insertion like?” PlannedParenthood.org (N.D.): Last accessed 2022 Mar 14.
- FDA. “Birth Control Chart.” (2021 Jun 14).
- Hubacher, David, Pai-Lien Chen, and Sola Park. “Side effects from the copper IUD: do they decrease over time?” Contraception 79.5 (2009): 356-362.
- Hall, Alexandra M., and Beth A. Kutler. “Intrauterine contraception in nulliparous women: a prospective survey.” Journal of Family Planning and Reproductive Health Care 42.1 (2016): 36-42.
- Maguire, Karla, et al. “Accuracy of providers’ assessment of pain during intrauterine device insertion.” Contraception 89.1 (2014): 22-24.